Erlinda Oracion on why WFSA’s Safety and Quality of Practice Committee developed the M&M tool kit.
Patient safety is a primary concern worldwide, and studies indicate that one in every 300 patients is at risk of harm during healthcare. In the case of such injury, hospitals hold Morbidity and Mortality (M&M) meetings to analyze adverse cases, identify root causes, and improve processes and patient safety. However, many hospitals in lower- and middle-income countries (LMIC) lack this essential review mechanism due to a lack of familiarity with the process or insufficient human resources. In some smaller hospitals, only one anaesthesia provider may be available to handle the surgical workload.
WFSA’s Safety and Quality of Practice Committee launched the Mortality and Morbidity Tool kit project to address this issue. The project aims to provide frontline staff, particularly anaesthesiologists, with an authoritative and adaptable resource to analyze patient morbidity and mortality events and improve patient care. The toolkit includes open-source techniques, open-access design, and technical and implementation resources to help hospitals implement M&M meetings.
The tool kit was developed after an extensive needs-analysis survey conducted in five LMICs and a group consensus of the committee members. It also includes background reading materials to guide readers on essential topics for advancing patient safety and risk management. Each chapter provides a suggested reading list for deep reflection and further self-learning to support optimal care delivery.
Overall, the Mortality and Morbidity Tool Kit is an essential resource for healthcare providers to analyze patient morbidity and mortality events, identify underlying causes, and improve patient care. This toolkit is particularly crucial in LMICs where the peer review mechanism still needs to be implemented due to unfamiliarity with the process or lack of human resources. With its collection of authoritative and adaptable resources, the toolkit offers practical approaches to address critical issues related to patient safety and risk management.
What are M&M Meetings?
Mortality and morbidity (M&M) meetings are regular review meetings held within healthcare institutions to analyze cases where patients experienced adverse outcomes, including death (mortality) or illness (morbidity). These meetings aim to identify the root causes of adverse events, discuss how to improve patient safety, and prevent similar incidents.
Mortality and morbidity meetings involve a multidisciplinary team of healthcare providers, such as physicians, nurses, and other staff members involved in the patient’s care. They also discuss any ethical or legal concerns related to the case. These meetings are vital to quality assurance and risk management in healthcare institutions.
Medical professionals attend these meetings to review and discuss patient cases that result in adverse outcomes or unexpected events. The conferences allow healthcare professionals to learn, share experiences, and collaborate to enhance patient care and safety. By examining cases where patients experience adverse outcomes or complications, healthcare providers can identify areas for improvement in clinical practices, procedures, and systems.
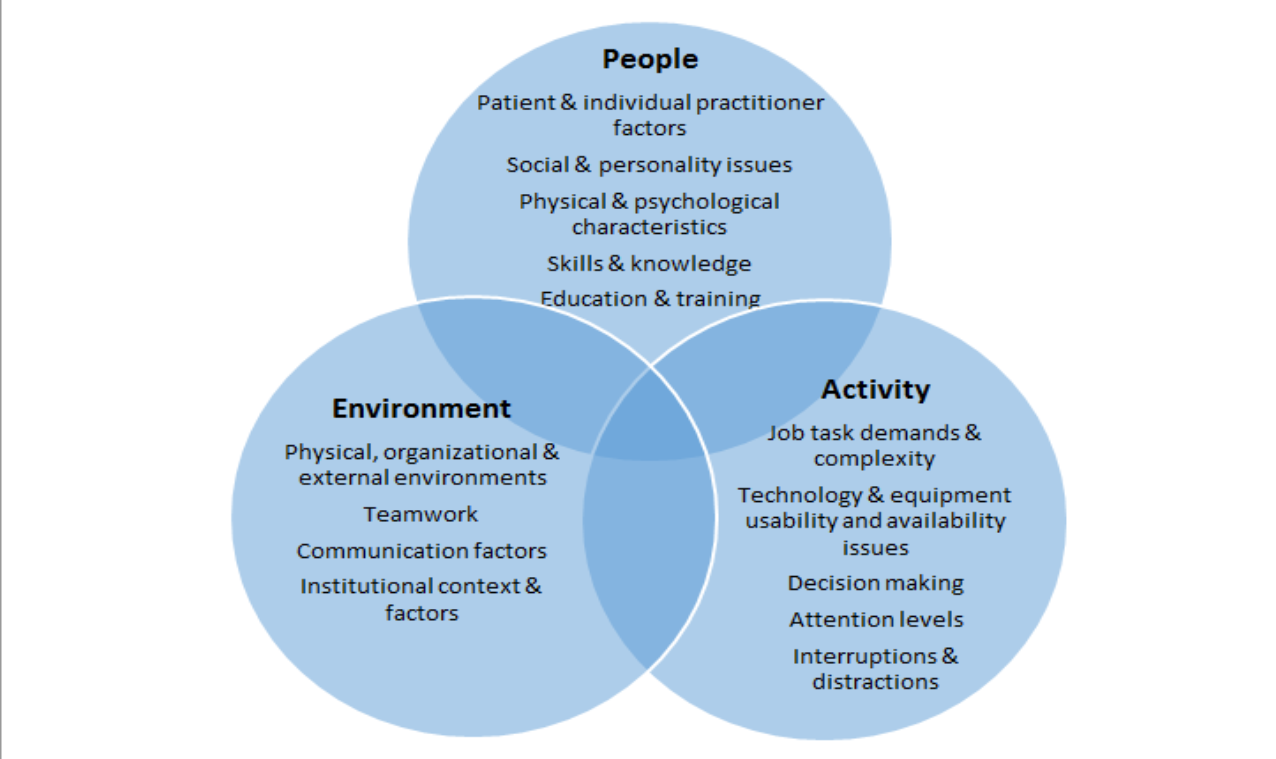
During the meetings, the team discusses the patient’s medical history, the events leading up to the adverse outcome, the actions taken by the healthcare providers, and the factors contributing to the outcome. The discussion may involve analyzing errors, identifying gaps in knowledge or skills, and discussing strategies to prevent similar incidents in the future.
Mortality and morbidity meetings promote a culture of learning, quality improvement, and patient safety within the healthcare team. The meetings help foster a supportive environment where individuals can openly discuss and learn from mistakes or adverse events without fear of blame or judgment.
Why is it essential to introduce M&M meetings to hospitals in LMICs?
Introducing Mortality and Morbidity (M&M) meetings in hospitals of LMICs is crucial to improving the quality of healthcare delivery and mitigating potential patient risks.
In many LMICs, healthcare providers face numerous challenges, such as inadequate infrastructure, limited resources, and insufficient training. These challenges can lead to poor clinical outcomes and increased morbidity and mortality rates. By introducing M&M meetings, healthcare providers can identify the root causes of adverse events, discuss how to improve patient safety and prevent similar incidents from happening in the future.
M&M meetings allow healthcare providers to reflect on their practices, share experiences and knowledge, and collaborate to enhance patient care and safety. In LMICs, where resources are limited, M&M meetings can be an effective and low-cost tool for quality assurance and risk management in healthcare institutions.
Introducing M&M meetings in LMICs can also help foster a culture of learning, quality improvement, and patient safety within the healthcare team. This can lead to improved clinical outcomes, enhanced patient satisfaction, and increased trust in the healthcare system. There are several reasons why introducing M&M meetings to hospitals in LMICs is essential:
- Patient safety: By examining adverse events and discussing the contributing factors, M&M meetings help identify potential risks and vulnerabilities in the healthcare system. This enables healthcare professionals to develop strategies and interventions to prevent similar incidents from occurring in the future, ultimately improving patient safety in LMIC hospitals.
- Quality improvement: M&M meetings provide a platform for healthcare professionals to analyze adverse outcomes and identify areas for improvement in clinical practices, procedures, and systems. In LMICs, where resources may be limited and healthcare systems may face unique challenges, M&M meetings can help identify specific areas where interventions can be made to enhance the quality of care.
- Learning culture: M&M meetings create a culture of continuous learning and professional development among healthcare professionals. By openly discussing cases and sharing experiences, knowledge, and lessons learned, healthcare providers can enhance their skills and knowledge base. This can improve clinical decision-making, patient outcomes, and a more robust healthcare workforce.
- Collaboration and teamwork: M&M meetings allow multidisciplinary teams to come together and collaborate. In LMICs, where healthcare delivery often involves multiple healthcare providers with different specialties, M&M meetings can foster collaboration, communication, and teamwork among these professionals. This can result in improved coordination of care and better patient outcomes.
- Research and data collection: M&M meetings can serve as a valuable data source for research and quality improvement initiatives. By systematically reviewing cases and collecting data on adverse events, healthcare professionals can contribute to the knowledge base and generate evidence for interventions and policy changes in LMIC settings.
Overall, introducing M&M meetings to hospitals in LMICs can improve the quality of care, enhance patient safety, foster a learning culture, promote collaboration, and generate valuable data for research and quality improvement initiatives.
Who is the M&M tool kit for?
The M&M toolkit is designed primarily for healthcare professionals involved in M&M meetings, including doctors, nurses, surgeons, specialists, and other healthcare providers. These meetings are typically held to review and discuss adverse events and unexpected outcomes.
Apart from healthcare professionals, the toolkit can also benefit hospital administrators, quality improvement teams, and patient safety officers who organize and facilitate M&M meetings.
Medical students, residents, and trainees learning and developing their clinical skills can also benefit from the M&M tool kit. It provides them with resources to understand the importance of M&M meetings and how to contribute to the discussions effectively.
In conclusion, the M&M tool kit guides healthcare professionals and teams in conducting meaningful and productive M&M meetings, regardless of their experience level or specialty.
How should the M&M tool kit be used?
The M&M tool kit is highly recommended for conducting productive mortality and morbidity (M&M) meetings. It provides healthcare professionals with a structured framework and resources to aid in reviewing and discussing adverse events and unexpected outcomes.
The toolkit comprises templates for organizing M&M meetings, guidelines for effective communication, and tools for analyzing data and identifying areas for improvement. It is designed to be flexible and adaptable to different healthcare settings and specialties.
Ultimately, the M&M tool kit aims to support healthcare professionals and teams conducting M&M meetings focusing on patient safety and quality improvement.
To use the toolkit effectively, healthcare professionals and teams should follow these steps:
- Please get familiar with the toolkit: Review the contents of the toolkit and understand its purpose, structure, and resources.
- Establish a process: Establish the logistics and process for conducting M&M meetings in your healthcare setting. This may include scheduling regular meetings, identifying a facilitator or chairperson, and selecting cases for presentation.
- Select suitable cases: Identify appropriate cases for discussion during M&M meetings, such as adverse events, unexpected outcomes, near misses, or issues with significant learning opportunities. Ensure proper consent and confidentiality measures are in place when discussing patient cases.
- Present cases: Use the toolkit’s resources and templates to structure the presentation of each case. This may include providing relevant patient information, describing the clinical course, highlighting critical events, and analyzing contributing factors. Encourage a multidisciplinary approach to case presentations, involving input from various healthcare professionals involved in the patient’s care.
- Analyze and discuss: Facilitate a thorough analysis and discussion of each case during the M&M meeting. Encourage open and honest dialogue, focusing on identifying factors contributing to the adverse outcome, discussing potential areas for improvement, and sharing knowledge and experiences. Use the toolkit’s resources, such as checklists or frameworks, to guide the discussion and promote systematic analysis.
- Develop action plans: Collaboratively develop action plans based on the insights and recommendations generated during the M&M meeting. These action plans should outline specific interventions or changes that can be implemented to prevent similar incidents. Assign responsibilities and timelines for implementing the action plans.
- Follow-up and evaluation: Monitor the progress of action plans and evaluate their effectiveness. Regularly review and discuss the outcomes of implemented interventions during subsequent M&M meetings. Continuously assess the impact of M&M meetings on patient safety, quality improvement, and the learning culture within the healthcare setting.
Remember, while the M&M tool kit is a helpful guide, it is essential to adapt its contents to the specific needs and context of your healthcare setting. Regular assessment and updating of the toolkit are necessary to ensure it remains relevant and effective in supporting your M&M meetings.
What effect do you hope the M&M tool kit will have on anaesthesia departments globally?
The M&M toolkit is expected to help anesthesia departments worldwide conduct meaningful M&M meetings that promote patient safety and quality improvement. By providing a structured framework and resources, the toolkit can support healthcare professionals in identifying areas for improvement, implementing changes, and preventing similar incidents in the future. Ultimately, it is expected to contribute to a culture of learning, collaboration, and continuous improvement within anesthesia departments.
There are several potential benefits to implementing the M&M toolkit in anesthesia departments globally. First, it can improve patient safety by helping departments identify and address potential risks and vulnerabilities in their practice. By analyzing adverse events and unexpected outcomes, departments can implement targeted interventions and protocols to prevent similar incidents.
Second, the toolkit can enhance the quality of care by facilitating the review and analysis of cases. This can help anesthesia departments identify areas for improvement and optimize their care processes, leading to better patient outcomes and increased patient satisfaction.
Third, the M&M toolkit can foster a culture of continuous learning and professional development within anesthesia departments. By openly discussing cases, sharing experiences, and analyzing errors, anesthesia professionals can enhance their skills, knowledge, and decision-making abilities, ultimately improving patient care.
Fourth, the toolkit can promote collaboration and communication among multidisciplinary teams within anesthesia departments. By working together to analyze cases, share insights, and develop action plans, anesthesia professionals can improve care coordination, enhance teamwork, and provide better patient care.
Finally, the M&M toolkit encourages data collection on adverse events and unexpected outcomes. This data can contribute to research efforts, allowing anesthesia departments to contribute to the evidence base and inform best practices globally.
Overall, the M&M toolkit has the potential to lead to improved patient safety, enhanced quality of care, a culture of continuous learning, collaboration among healthcare professionals, and the generation of valuable research and evidence-based practices in anesthesia departments worldwide.