WFSA Project Manager Amelia Crowther’s photo diary of a scoping trip to Malawi to help shape a new specialised programme
By Amelia Crowther
In May 2023, I began my travels in Malawi by visiting five district hospitals. Feedback from these visits will help develop a new long bone fracture (LBF) programme, scheduled to pilot in Blantyre in December 2023.
LBF is a common injury in Malawi. Road traffic accidents, a significant cause of LBF, are widespread – yet specialised care physicians are low, with only 8 physician anaesthesia providers for a population that exceeds 17 million.
The new LBF programme, funded by Johnson & Johnson Foundation and the result of a partnership between WFSA, AO Alliance, Kids OR, Lifebox and the Malawian Ministry of Health, looks to strengthen LBF anaesthesia and trauma care services by delivering courses in essential pain management (EPM), primary trauma care and clinical leadership.
The visits to the five hospitals were planned to provide insight into current anaesthesia practice for LBF management, ensuring the new course is tailored to the needs of the anaesthesia community working in both rural and urban settings in Malawi.
Day 1-3: visits to five district hospitals
The programme inception visits were conducted with our in-country lead for the project, Dr Stella Singatiya Chikumbanje, the Secretary of the Malawian Society of Anaesthesiologists and Chief Anaesthesiologist at Queen Elizabeth Central Hospital (QECH).


On the first day, we drove to Dowa District Hospital to meet with Clemencia Chiwaya, the head Anaesthesia Clinical Officer (ACO) – due to the low number of anaesthesiologists in Malawi, it is not unusual for Anaesthesia Clinical Officers to lead on anaesthesia practices in their hospitals.
On day two, we drove to Salima District Hospital near Lake Malawi to meet ACO lead Thandie Munthali, then along the Mozambique border to Ntcheu District Hospital to meet ACO lead John Chikaonda.
With all the ACOs, we used a new survey developed by WFSA clinicians – specifically for the LBF project – to identify strong areas in LBF management, as well as those requiring skill training and knowledge improvement in their hospitals.

Questions on the survey explored current practices for LBF, including the management of trauma cases in the ER, the use of regional anaesthesia in fracture management, and the analgesia usually given pre-, intra- and post-operatively for LBF.
We also conducted a baseline survey at the hospitals, which included the Anaesthesia Facility Assessment Tool (AFAT). The AFAT helps to gather data about the anaesthesia workforce, equipment, medicines and practice at the facility level, so is useful in better understanding anaesthesia capacity and facility provision gaps.
On the final day, we visited Machinga District Hospital in Liwonde to speak with ACO lead Cecilia Kwezani and observe a caesarean section. Then, we visited QECH when we arrived in Blantyre – our final stop for the inception visits.
Day 4: planning for the EPM course
After the hospital inception visits, I travelled to Blantyre to sit in on two Essential Pain Management (EPM) courses and an EPM Training of Trainers (ToT) course. Run in over 55 countries, EPM brings together local health workers to improve pain knowledge and help implement a simple framework for managing pain.

EPM courses have taken place in Blantyre before in 2014 and 2016 – Rose Kapenda (third from right), now a EPM trainer, was trained by Dr Karen Gilmore (first on right) on the EPM ToT course in 2016.
Volunteers from Kenya, Rwanda and the UK joined with the local trainers from Lilongwe and Blantyre to plan sessions and presentations for the upcoming EPM courses.
Many of the attendees of this Blantyre EPM course will be attending the LBF pilot course in December 2023, so the faculty ensured the schedule delivered traditional EPM skills, with an additional focus on LBF management.
Day 5: the first EPM workshop
37 participants from QECH attended the first one-day EPM workshop. The multidisciplinary participants included anaesthetic registrars, orthopaedic registrars, clinical officers, and nurses.
The group engaged in presentations and discussion sessions on topics including assessment of pain severity, classification of pain, treatment of pain, barriers to pain management, and the ‘Recognise, Assess, Treat’ (RAT) model.
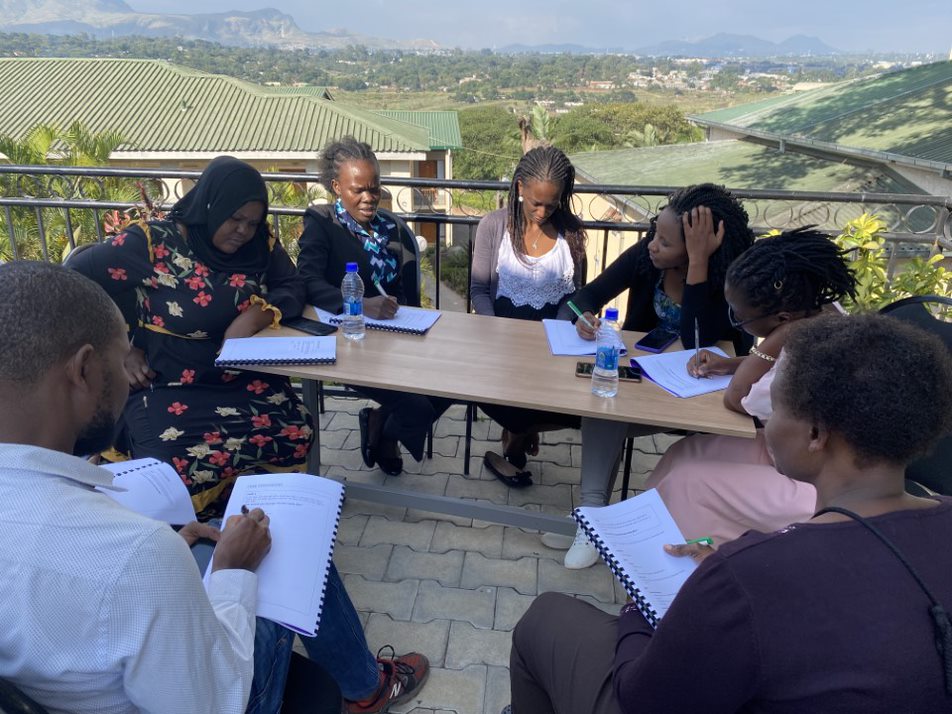

Day 6: EPM Training of Trainers course
10 multidisciplinary participants from the EPM course were selected to attend a half-day instructor Training of Trainers (ToT) course. The EPM course promotes early handover of teaching to local instructors, to encourage educational sustainability and help develop local pain management champions.
The faculty covered lecture planning, gave tips on presentation skills and highlighted ways to engage EPM participants in a discussion. In the afternoon, they visited QECH to meet anaesthesia leads and discuss current pain management practices.
The 10 newly-trained ToTs went on to teach the EPM course in Blantyre the next day.


Day 7: the second EPM workshop

Led by the newly trained ToTs, the second one-day EPM workshop was attended by 43 multidisciplinary participants from QECH and the other four district hospitals that are part of the LBF project.
Anaesthesia and orthopaedic clinical officers and nurses – including the four ACOs from the hospital inception visits – from Dowa, Salima, Ntcheu, and Machinga will be mentored to champion pain management in their districts. They will go on to play a vital role in the sustainability of future courses, including the upcoming course on long bone fracture.
The LBF pilot course is scheduled to run in Blantyre in December 2023. WFSA would like to thank the Johnson & Johnson Foundation for their continued support.
Further Reading
Essential Pain Management – EPM Courses
Epidemiology of fractures and their treatment in Malawi
You can help anaesthesia professionals like those training in Malawi attend WCA 2024 through the WCA Scholarship Programme
Title image: EPM course participants and faculty