Dr John Severinghaus, who passed away on 2 June 2021, pioneered the foundations for many anaesthesia technologies still in use today. Dr Severinghaus was a great friend of WFSA and supporter of Fund a Fellow and will be greatly missed.
As the longest-standing faculty member of their Department of Anesthesia and Perioperative Care UCSF reflect on a remarkable life and his essential work.
The Master Tinkerer and the Blood-Gas Analyzer

John Severinghaus was originally a physicist who had spent the latter part of World War II designing radar. It was only after the war that he turned his attention to medicine, receiving his MD from Columbia and, in 1952, beginning an anesthesia residency at the University of Pennsylvania.
At Penn, a portable paramagnetic oxygen analyzer fascinated the man his friend Ted Eger called “a master tinkerer.” Using himself as “human servo” he measured the uptake of nitrous oxide at the beginning of an anesthetic, keeping the oxygen at 20% and closed system volume constant using flow meters. It was the first measurement of the uptake of an anesthetic in a human, a modest beginning to a crucial medical advance.
Two years later at a conference, Severinghaus heard physiological chemist Richard Stow, describe a carbon dioxide electrode he had developed, but could not stabilize. “A few days later, I built a Stow type CO2 electrode using a bulb type Beckman pH electrode, a silver wire with an AgCl coat, and a rubber glove membrane. My contribution was pretty simple,” said Severinghaus. “Add soda.”
The next step came in early 1956, when at an informal meeting of respiratory physiologists that Severinghaus convened, a liver enzyme chemist named Leland Clark pulled from his pocket a polarographic O2 electrode with a polyethylene membrane. Within days, Severinghaus had begun the design of a water bath containing the PCO2 and PO2 electrodes, with a stirred cuvette for the Clark electrode. “Clark’s electrode was the key discovery,” said Severinghaus. “Fifty years later, every blood gas analyzer contains a Clark type electrode.”
Finally, shortly after arriving at UCSF and with the help of his friend and colleague Freeman Bradley, Severinghaus added a pH electrode to this evolving device, creating the first three-function blood gas analyzer. By 1960, he had built and installed a clinical blood-gas analyzer in the Moffit Hospital OR Suite.
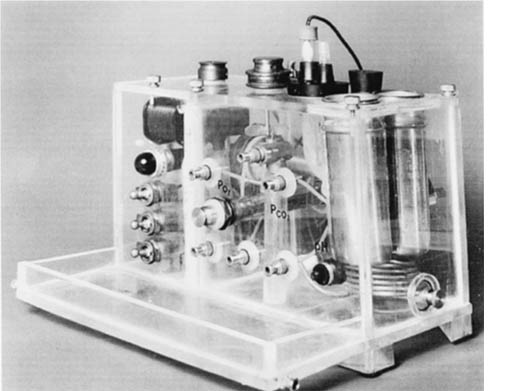
“I initially failed to foresee the immense clinical potential of blood gas analysis,” said Severinghaus, who developed it for his laboratory pulmonary studies. Yet because of the way it allows physicians to safely monitor heavily sedated or ventilated patients, today no operating room goes without the device. His original three-function analyzer resides in the Smithsonian as part of an exhibit on the conquest of pain.
Discovering and Exploring the Brain’s Carbon Dioxide Sensor
Over the years, the Severinghaus lab became a virtual petri dish for leading researchers and important research. Internist Robert Mitchell joined the lab in 1958 and would share the space for the next thirty-two years.
Mitchell’s greatest contribution was his discovery, with Hans Loeschke, of the medullary area that regulates blood PCO2, keeping spinal fluid pH constant. Today, when patients with conditions like COPD have abnormal CO2 levels, the results are understood in the context of Mitchell’s chemoreceptors.
That finding also “promised to explain a physiologic mystery,” said Severinghaus. “Why is it that people acclimatized to high altitude continue to over-breathe for days after descending?”

To answer that question, Severinghaus, Mitchell and two colleagues piled in a car and made their way to UC’s Barcroft Lab in the White Mountain range, east of the Sierras. They lugged a blood-gas analyzer up there and volunteered to have their own spinal fluid tapped. What they found was the first confirmation that rapid changes of cerebrospinal fluid acid-base explain the mysteries of acclimatization.
The Big MAC
Ted Eger first became interested in the uptake and distribution of inhaled anesthetics after hearing a talk by John Severinghaus when both were still at Iowa. He spent an hour afterwards arguing with Severinghaus, telling him he surely was wrong (he wasn’t). Later, during a stint in the Army, Eger devised a handwritten iterative equation on how anesthetics move into the lungs and tissues of the body. Anxious to continue his work in this area, in 1960 he arrived at UCSF to become a fellow in the Severinghaus lab.
At the time, various drug companies were competing to improve upon halothane, which had revolutionized anesthesia. One day in Severinghaus’s small, cramped lab overflowing with experiments of different kinds, Severinghaus handed Eger a bottle of something called halopropane. “He asked me to find out if it was any good,” said Eger. “And when I asked him how, exactly, he shrugged and told me I would figure it out.”
That bottle of halopropane would prove useless as an anesthetic, but it was the perfect vehicle for Eger to learn how to compare one anesthetic to another. This led to his discovery of minimum alveolar concentration (MAC). In parallel, he enlarged his research on uptake and distribution. The work on MAC and pharmacokinetics was unparalleled in its contribution to understanding inhaled anesthetics’ effect on all aspects of human physiology: breathing, circulation, cerebral function, neuromuscular control, and kidney and liver well-being.
Adapted from the original article on https://anesthesia.ucsf.edu/news/john-severinghaus-pioneer-anesthesia-and-medicine-has-passed-away-may-6-1922-june-2-2021